——————————————————–
Information and Pictures on Granuloma, a sexually transmitted disease. Information includes symptoms, diagnosis, treatment, transmission, prevention and other general information.
——————————————————–
Granuloma Information
Granuloma inguinale is also known as:
- Donovanosis
- Granuloma venereum
Granuloma inguinale is a sexually transmitted disease (STD) occurring more frequently in males. It is caused by a bacterial species usually found in the tropics and subtropical areas. It is a chronic condition once contracted and can be mildly contagious.
Very few cases are reported in the United States. The main target group is homosexual men aged between 20-45.
Symptoms
One week to several months (average incubation 8-80 days) after the initial exposure to the infection, lumps or blisters appear in the genital area. These slowly enlarge into open sores, similar to those caused by chancroid, syphilis or herpes.
These mainly appear on:
- the mucous membranes around the genital area,
- the skin.
The sores spread along warm, moist folds of skin from the groin to the genitals and anus.
Although discomfort increases as the infection progresses, the sores are not necessarily painful.
In men
Lesions first appear:
- on the head of the penis,
- on the shaft of the penis.
In women
Lesions first appear:
- at the entrance to the vagina,
- at the inner labia.
If untreated, the sores grow larger and spread throughout the groin, which can cause:
- abscesses,
- cancer (in rare cases),
- intestinal and rectal symptoms,
- secondary infections.
Other symptoms:
- Swelling of the lymph nodes.
Inguinal nodes spread infection into overlaying tissues which can cause:
- abscess formation (pseudobubo),
- ulceration of the overlaying skin,
Untreated infections can:
- persist and slowly spread,
- resolve spontaneously.
——————————————————–
Photos of Granuloma SymptomsTransmission
Granuloma inguinale can be transmitted:
- if infected persons remain untreated and bacteria from lesions are present,
- through anal sex or oral-anal contact,
- through contaminated food or water,
- through sexual contact with an infected individual,
- through touching or scratching other parts of the body,
- when the disease is in its early stages and symptoms go unnoticed.
Re-infection and spreading of the infection can occur through:
- open wounds,
- skin abrasions.
- Blood tests, are used to determine that it is not another STD with similar symptoms.
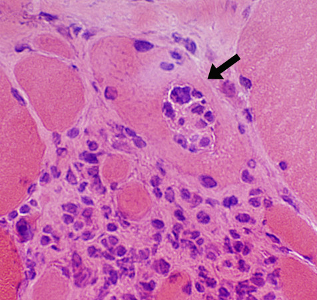
- Microscopic examination of cells from the edge of the sores.
- Tissue samples are collected by biopsy.
- Visual observation is made by an expert of the external symptoms.
Examination
- Cellular material is collected and placed onto a glass slide for examination under a microscope.
Biopsy
- Biopsies are best stained with silver stains, such as Warthin-Stary or Giemsa, Wright’s or Leishman stain.
Blood Tests
- Successful culture of the causative organism, Klebsiella granulomatis has been reported in human peripheral blood monocytes and in HEp-2 cells.
- Polymerase chain reaction (PCR) methods and serological tests are not yet routinely available.
Treatment
To eliminate the infection a two-week course of antibiotics is usually administered using:
- Azithromycin
- Ciprofloxacin, which has better bio-availability than Norfloxacin.
- Doxycicline is recommended based on trials carried out with older Tetracyclines.
- Erythromycin
- Gentamicin is recommended to patients whose lesions do not respond to other medication in the first few days.
- Minocycline
- Sulfamethoxazole
- Tetracycline
Sores:
- begin to clear within a week after treatment begins
- and will often heal completely within 3-5 weeks.
A minimum of 3 weeks’ treatment is recommended
Note:
The addition of proteolytic enzymes can improve the effectiveness of antibiotics.
Treatment during Pregnancy or Lactation
- Erythromycin has been used successfully in pregnant women.
Note
The following antibiotics are not recommended during pregnancy or lactation:
- Co-trimoxazole
- Doxycycyline,
- Gentamicin
- Norfloxacin
Children born to mothers with untreated genital lesions are at risk of infection and a course of prophylactic antibiotics is recommended.
Naturopathic Treatment
- Abstain from sexual activity while healing from this bacterial infection.
- Use direct, local, anti-microbial applications.
- Fortify the immune system to fight the infection and heal the body.
Dietary Recommendations
Include
- fresh fruits
- leafy green vegetables
- pure water
- whole grains
Avoid
- alcohol
- carbonated beverages
- fast foods
- fruit juice
- processed foods
- refined white flour, including pasta, bread, desserts
- sugar
Nutritional Supplements
Proteolytic enzymes:
- Bromelain 400mg
- Wobenzyme N five tablets 3-4 times a day not with meals
and
- Vitamin A
- Vitamin C 1,000 mg 3 times a day with meals
- Zinc 30 mg daily
——————————————————–
Herbal Treatment
- Goldenseal (Hydrastis Canadensis), strong infusion or poultice applied locally to sores
- Goldenseal (Hydrastis Canadensis)
- Vitamin A suppository
Other Treatment
- Warm sitz baths with several drops Tea Tree oil (Melaleuca alternifolia).
Vaginal douching using the following dried herbs, which have potent anti-microbial properties.
- Goldenseal (Hydrastis canadensis)
- Oregon Grape Root (Mahonia aqjuifolium)
Prevention
- Avoid oral/anal and unprotected penile/anal sex if sexually active.
- Carefully wash the genitals after sex.
- If you suspect you have come in contact with an infected person, contact your local STD Clinic, health professional or urologist immediately.
- Use latex condoms put on before sex and worn until the penis is withdrawn.
- Limit sexual relationships to a single, uninfected partner.
- Notify all sexual contacts immediately so they can obtain treatment if infected.
- To avoid re-infection, patients should be monitored until all symptoms have ceased.
Note
- Douching or urinating after sex does not prevent STDs.
Prognosis
If untreated the sores grow larger and spread throughout the groin and can cause:
- abscesses,
- cancer (in rare cases),
- intestinal and rectal symptoms,
- secondary infections.
Complications
- This condition can be spread to other parts of the body.
- Occasionally development of squamous carcinoma occurs.
- There can be extensive destruction and mutilation of the genital organs.
- Genital lymphoedema can occur (swelling of the lymph nodes).
- Hematogenous (related to the blood) dissemination to bone and viscera, particularly during pregnancy, can occur.
- Hemorrhaging can occur.
- Lesions can form in the ears of infected infants.
- Primary lesions of the mouth and cervix can form which are often mistaken for malignant lesions.
- Abscesses can form in the Psoas muscle in the loins and around the kidneys.
- Scars left by the sores may be precancerous, therefore annual medical checkups should be undertaken.
- Spinal cord compression cab occur.
Past infection does not make a person immune and there is no evidence of natural resistance.