Information and Pictures on Chancroid, a common sexually transmitted disease. Information includes symptoms, diagnosis, treatment, transmission, prevention and other general information.
Chancroid (Kan-kroid) is also known as:
- soft chancre
- venereal sore.
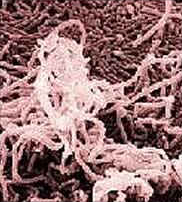
Chancroid ( human genital ulcer disease) is an STD caused by exposure to Haemophilus ducreyi. This is a small, gram-negative rod bacteria that occurs mainly in developing countries, especially in Africa, Asia and Latin America.
Infection from Chancroid related to Haemophilus ducreyi is decreasing in many areas. However infections related to Herpes simplex virus type-2 (HSV-2) are increasing.
Chancroid causies painful, irregularly shaped sores, but it is a localized infection which can be treated and cured and has no long-term effects.
The size can vary from 1-2 millimeters to several centimeters but is usually 1-2 centimeters in diameter.
The shape can be:
- irregular
- oval
- round
Unlike the chancre of syphilis:
- The chancroid ulcer edge is soft.
- The ulcer changes shape when the edges are squeezed.
Over 4,000 cases are reported annually, occurring mainly in younger adults, although it can affect any age.
Contents
Chancroid Symptoms
First signs of infection appear from 3-5 days and up to 2 weeks after contact. Usually a tender, raised bump develops where the bacteria entered the body:
- inside/outside the vagina or rectum
- occasionally on hands, thighs, mouth or on the penis.
Within 1-4 days the bump transforms into one or more shallow sores which break open and deepen, becoming:
- filled with pus
- inflamed
- painful
- ruptured.
The next stage may persist for several weeks and may result in:
- a painful open sore
- a purulent ulcer
- several lesions merging to form gigantic ulcers.
In over half of the untreated cases, the chancroid bacteria infect the lymph glands in the groin.
The lymph glands in the groin may:
- swell, creating a pus-filled bulge, known as a bubo
- enlarge until they burst through the skin
- drain continuously
- remain open
- become infected by other bacteria
- may be firm or unstable
- may rupture or ulcerate.
The typical chancroid bubo:
- Appears about 1-2 weeks after the ulcer forms.
- Is unilateral, spherical and painful.
In men:
- 1-4 sores on the penis may develop.
- Buboes appear in about 50% of male patients.
- The foreskin may swell.
The ulcers usually are found in:
- the prepuce near the frenulum
- coronal sulcus
- glans
Rectal sores may:
- bleed
- cause pain when defecating
In women:
- Buboes are uncommon in women.
- Sex may be painful (dyspareunia).
- Urination may be painful (dysuria).
- Painless sores can develop on the cervix.
- Several sores may develop around the vagina and rectum.
- There may be a vaginal discharge.
The ulcers usually are found on the:
- cervix
- entrance of the vagina, particularly the fourchette
- labia majora and minora
- peri-anal area.
Rectal sores may:
- bleed
- cause pain when defecating
Chancroid Transmission
Chancroid is transmitted through the skin by direct sexual contact with an infected individual through:
- anal sex
- oral sex
- vaginal sex
The infection is spread to other parts of the body by:
- minor abrasions
- physical contact
- rubbing
- scratching.
Other
- An uncircumcised man is more likely to contract the disease than a circumcised man.
- Any sexually active person can be infected with chancroid.
- If a person does not practice personal hygiene it is easier for the infection to be transmitted.
- It is more commonly seen in men than in women.
Risk Factors
- Contact between scraped or broken infected skin increases the likelihood of transmission.
- Ejaculation is not necessary for the infection to be spread.
- Even if using a condom, sores may be present on areas not protected by the latex. These can cause infection anywhere they contact receptive tissue.
- The bacteria are more likely to invade the sexual organs at the point of a pre-existing injury, such as a small cut or scratch.
More outbreaks occur in:
- drug users
- people with other STDs
- prostitutes and their clients.
Re-infection can occur from:
- minor abrasions
- open wounds.
The disease is not spread from person to person by casual contact such as:
- clothing
- door knobs
- eating utensils
- swimming pools
- toilet seats
- Mothers do not pass it on to babies at birth.
How is Chancroid Diagnosed?
Chancroid is usually diagnosed by:
- culture or biopsy
- gram stain
- microscopic examination of a smear sample taken from the patient’s sores.
Although the disease does not enter the bloodstream,a blood sample is usually taken to check for the presence of other STDs.
Culture:
- Diagnosis requires culturing H ducreyi on special culture medium that is not always available.
- The sensitivity is not higher than 75%.
- The bacterial specimens should be checked out immediately at the clinic or sent rapidly (within 4 hours) to the laboratory.
Gram Stain:
- Sensitivity range from 10-90%
- The classic description of H ducreyi is that of a ‘school of fish’ with small, pleomorphic, gram-negative rods.
- Has limitations in diagnosing chancroid.
Serology (blood test):
- Inability to distinguish acute from past exposure.
- Calcium alginate or plastic swabs should be used for collection of samples.
New techniques:
New ways of diagnosis are constantly being researched, such as:
- Antigen-detection techniques involving immuno-fluorescence or radio-isotopic probes.
- Detection of nucleic acid (DNA) by amplification techniques such as Polymerase Chain Reaction (PCR) which is 95% sensitive compared to a culture specimen.
Note:
The doctor or health professional should be advised if the patient has a history of HIV infection. HIV seropositivity can be responsible for an atypical presentation of chancroid.
HIV-infected patients have :
- a larger number of ulcers
- atypical ulcers and extra-genital lesions
- longer lasting ulcers
Screening for other possible causes of genital ulcerative disease should be arranged, particularly the diagnosis of:
- Donovanosis (Granuloma inguinale)
- Herpes simplex virus (HSV)
- Lymphogranuloma venereum (LGV) caused by a virus and spread by sexual intercourse and contaminated articles
- Treponema pallidum, the organism that causes syphilis.
Biopsy of lymph nodes may be required to exclude:
- Neoplasia (the presence of new growths or tumors).
Chancroid Treatment:
Buboes may need to be drained with a needle under local anesthetic.
Although treatment with antibiotics can cure the infection, strains are becoming more common that are resistant to:
- Ampicillin
- Chloramphenicol
- Penicillin,
- Tetracycline
Conventional Treatment:
Current treatment involves regular doses for up to two weeks of:
- Ciprofloxacin
- Erythromycin
- Trimethoprin
or a single dose of:
- Azithromycin
- Ceftriaxone
Chancroid Drug Information
Azithromycin (Zithromax):
- Treats Chlamydia and Gonorrhoeaea infections of the genital tract.
- Treats mild to moderately severe infections caused by susceptible strains of microorganisms.
Contraindications:
- Concurrent Pimozide treatment (sudden death may occur)
- Hepatic impairment
- Hypersensitivity
- Interactions with other substances
Decreased effects if taking:
- Aluminum antacids
- Magnesium antacids
Increased toxicity of:
- Digoxin
- Theophylline
- Warfarin
If taking Cyclosporine there is an increased risk of:
- Nephrotoxicity
- Neurotoxicity
Side Effects:
- Bacterial or fungal overgrowth with prolonged use
- Cholestatic jaundice
- May increase hepatic enzymes
- Site reactions can occur with IV route.
Caution
Care should be used when dealing with patients:
- who are debilitated
- who are geriatric
- who are hospitalized
- who have pneumonia
- or during pregnancy. It has not been established if it is safe for pregnant and lactating women.
Ceftriaxone (Rocephin):
- Stops bacterial growth by binding to one or more penicillin-binding proteins.
Contraindications:
- hypersensitivity
- interactions with other substances
Probenecid may increase levels of:
- Ceftriaxone
Nephrotoxicity increases if taking:
- Aminoglycosides
- Ethacrynic Acid
- Furosemide
During Pregnancy
- It is thought to be safe but benefits must outweigh the risks.
Caution:
- Dosage should be adjusted if there is renal impairment.
- It should not be used by breastfeeding women.
- It should not be used if allergic to penicillin.
Erythromycin is used to inhibit:
- bacterial growth
- RNA-dependent protein synthesis.
Note:
Erythromycin is used to treat patients allergic to:
- Cephalosporines
- Quinolones
Contraindications:
- hepatic impairment
- hypersensitivity
- interactions with other substances
Increases toxicity of:
- Carbamazepine
- Cyclosporine
- Digoxin
- Theophylline
Anticoagulant effects potentiated of:
- warfarin
Increased risk of Rhabdomyolysis if taking:
- Lovastatin
- Simvastatin
Side-Effects:
- adverse gastro-intestinal effects
- cholestatic jaundice may occur
During Pregnancy:
- thought to be safe but benefits must outweigh the risks
Caution:
-
-
- in liver disease
-
Discontinue if the following occurs:
- abdominal colic
- fever
- malaise
- nausea
- vomiting
Ciprofloxacin (Cipro)
Is a bactericidal antibiotic that is used to inhibit:
- bacterial DNA synthesis and growth
Contraindications:
- hypersensitivity
- should not be used for children and adolescents under 18
- interactions with other substances
Serum concentrations may be increased if taking:
- Probenecid
Serum levels may be reduced if taking:
- antacids,
- iron salts
- zinc salts
If taking Cimetidine it may interfere with the metabolism of:
- Fluoroquinolones
Reduces the therapeutic effects of:
- Phenytoin
Increases the toxicity of:
- Caffeine
- Cyclosporine
- Digoxin
- Theophylline
Note
- :
- Digoxin levels should always be monitored.
- If it is necessary to take antacids always have them 2-4 hours before or after taking Fluoroquinolones.
- The effects of anticoagulants may be increased.
During Pregnancy:
- Ciprofloxacin is contraindicated for pregnant and lactating women.
Caution:
-
-
- Dosage should be adjusted if there is renal function impairment.
- Superinfections may occur with prolonged or repeated therapy.
- The addition of proteolytic enzymes to antibiotic treatments has been shown to improve the effectiveness of the antibiotics.
Follow-up:
An examination should be carried out 7 days after starting treatment. If there is no obvious improvement, several possibilities should be considered:- Swelling and inflammation of the lymph glands takes longer to heal than ulcers.
- Large ulcers take more time to heal than small ulcers.
- Check to see if the course of antibiotics was not followed properly.
- The H ducreyi strain may be resistant to the prescribed antibiotic.
- The person may have HIV, making healing slower.
- Check for the presence of another STD or illness.
In HIV-positive patients:
- Cure rates using standard antibiotic treatments are lower than in the general population.
- Longer treatment courses are usually necessary.
Naturopathic Treatments:
- Practice abstinence from sexual activity while healing from the bacterial infection.
- Fortify the immune system to increase its ability to fight infection and heal.
Chancroid can be difficult but not impossible to cure with natural treatments, if you are consistent and patient.
Dietary Recommendations
Include:
- essential fatty acids, such as olive oil, nuts
- fish and poultry
- flax seed, (linseed) oil
- fresh fruits and vegetables
- organic foods where possible
- plenty of fresh water ( drink as much as possible)
- whole grains
Avoid:
- alcohol
- carbonated beverages
- dairy products
- fruit juice
- refined white flour, such as pasta, bread, desserts
- sugar
Nutritional Supplements:
- Proteolytic enzymes:
- Bromelain 400mg
- Wobenzyme N five tablets three to four times a day away from meals
and
Herbal Treatments:
- Goldenseal (Hydrastis canadensis), strong infusion or poultice applied locally to sores
- Goldenseal (Hydrastis)/Vitamin A suppository
Other Treatments:
- warm sitz baths with several drops tea tree oil (Melaleuca alternifolia) added.
vaginal douche using one or both of the following herbs which have potent anti-microbial properties: Goldenseal (Hydrastis canadensis) and Oregon Grape Root (Mahonia aqjuifolium)
Prevention of Chancroid Infection
Risk Factors:
- Douching or urinating after sex does not prevent STDs.
- Exposure of skin and mucus membranes with a high risk partner.
- If there are any signs or symptoms of chancroid, abstain from sex until the infection is cured.
Help Factors:
- Carefully wash the genitals with antibacterial soap immediately after sex.
- Limit one’s sexual relationships to a single, uninfected partner.
- Practice safe sex.
- Use latex condoms or gloves put on before sex. Dispose of them responsibly immediately after sexual contact.
Other Precautions:
- Notify all sexual contacts immediately so they can obtain examination and treatment.
- Patients should be tested for syphilis and retested 3 months later if initial test result is negative.
- Testing should be repeated 3 months later if the initial test results are negative.
- Visit your local STD clinic, hospital, doctor or urologist immediately, if you have come in contact with chancroid.
Chancroid Prognosis:
- Chancroid does not seem to have any adverse effects on pregnancy or the fetus.
Complications of Chancroid:
- Inflammation and partial loss of tissue, particularly of the glans, penis and prepuce may occur.
- Buboes may rupture and take months to heal.
- Fistulous tracts, abnormal tube-like passages within the body tissues, may form.
- Tightness of the foreskin may occur.
- Scarring from extensive infection or from burst buboes may occur.
- Untreated chancroid often results in ulcers occurring on the genitals, which can persist for weeks or months.
Risk Factors:
- People with open chancroid sores are especially vulnerable to other STDs.
- Re-infection can occur as the body does not build up any natural resistance.
In less than 10% of cases sores may return and these may be caused by:
- improper use of medication,
- an incomplete cure,
- re-exposure to the bacteria through recently healed skin,
- or a weakened immune system.
Note
It has been found that the genital ulcers of chancroid have:- been associated with the sexual transmission of the HIV virus,
- and occurred as outbreaks in populations with a high incidence of HIV-1 infection.
-

