Contents
Lymphogranuloma Information & Pictures
A condition caused by a sexually transmitted organism. Lymphogranuloma information including symptoms, diagnosis, treatment, transmission, prevention and other general information.
Lymphogranuloma inguinale is also known as:
- Lymphogranuloma venereum (LGV)
- Nicholas-Favre Disease
- Sixth Venereal Disease
- Tropical Bubo
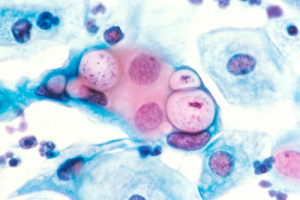
Lymphogranuloma inguinale is an infection of the lymph tissue in the genital area caused by a strain of Chlamydia trachomatis, the bacteria that produce Non-gonococcal Urethritis (NGU). The disease occurs most often
- Africa
- Central America
- South America
- Southeast Asia
- The Caribbean
Lymphogranuloma inguinale infects on average about 250-400 people a year in the United States.
Lymphogranuloma Symptoms
Lymphogranuloma inguinale has three stages:
Stage 1
- a small, painless sore similar to a pimple, blister/lesion/soft bump develops at the point where the bacteria entered the body (usually the penis or vagina) that often goes unnoticed
- some people do not experience this and if they do, healing is usually rapid without scarring
- the infection then spreads to the lymph nodes in the groin area and from there to the surrounding tissue, where it causes painful swelling closest to the point of infection
- discharge from the penis or vagina from 3-30 days after exposure
Lymphogranuloma inguinale is found on: In Males
- the coronal sulcus of the penis
In Females
- the cervix
- the fourchette (fold of skin at the posterior margin of the vulva)
- the posterior vaginal wall
- the vulva
Lesions have also occurred:
- in the oral cavity (tonsils)
Stage 2 (1-2 weeks after initial symptoms appear)
- inflammation and swelling of lymph nodes and surrounding tissue
- lymph nodes closest to the infection continue to swell until a pus-filled bulge is created, called a bubo
- throbbing pain and fever
The buboes can:
- grow very big, until the skin covering them turns blue
- open through the skin, drain continuously and remain open (about 30% of cases)
- become infected by other bacteria
In Women the buboes may cause:
- erosion of the skin and tissue between the legs
- erosion of the vagina or rectum walls
- painful swelling in the groin
Buboes near the anus may cause:
- discharge from the rectum
- infection of the penis
- infection of the rectum
- swelling, bleeding and erosion of the lining of the rectum, which can spread upwards into the colon
- the rectum may swell almost shut
Buboes in the penis or vagina
- affect the nodes on either or both sides of the groin
- may cause sores or pus-filled sacks to develop on the genitals
Buboes in the throat affect
- the nodes in the jaw and neck
Stage 3
With Lymphogranuloma the process of infection and healing can be accompanied with scar tissue where fibrosis has formed. This scarring can lead to a range of strictures, lymph obstructions and chronic edema. This later stage of the condition where edema and fibrosis is present is known as the final and 3rd stage of Lymphogranuloma. These developments in the tissue are generally permanent. —–
Lymphogranuloma Transmission
Lymphogranuloma inguinale is spread by direct sexual contact with the:
- genitals
- mouth
- rectum
Note
- an individual is infectious for as long as the lesions remain active
- ejaculation is not necessary for the disease to be spread
- the germ is passed from partner to partner as long as there are sores
- the infection is spread by unprotected sexual contact
In Pregnancy and Birth Infected mothers can transmit the disease to their babies at birth It can not be spread from person to person by casual contact, such as:
- clothing
- door knobs
- eating utensils
- swimming pools
- toilet seats
Lymphogranuloma Diagnosis
Diagnosis is usually ascertained by:
- a blood test
- a sample of the discharge for a culture test
- visual observation
to rule-out or check for other STDs such as:
As Chlamydiae are intra-cellular organisms, samples must contain cellular material. This can be obtained:
- by aspiration from fluctuant lymph nodes or buboes with a needle
- from the base of the ulcer
- from rectal tissue
Methods
- ost methods are usually unable to distinguish Lymphogranuloma inguinale strains from other Chlamydial strains
Culture Test Culture on Cycloheximide treated cells from suspected lesions is the most specific method. The method:
- has a sensitivity of 75-85%
- has a sensitivity of 30-50% in the case of bubo aspirates (the pus has a toxic effect on the culture cells)
- is expensive
- is labor intensive
- is not not readily available
Direct Immuno-fluorescence (DIF) Material from a suspected lesion is used to detect Chlamydia trachomatitis. A fourfold rise in antibodies (both IgM and IgG) usually shows active infection. This method:
- is labor intensive
- is sensitive
- is only performed in a few specialized laboratories
- requires the proper expertise for interpretation
Enzyme immunoassay (EIA) This method is suitable for ulcer scrapes or bubo aspirates, but not for rectal samples. The method:
- is convenient
- is objective
- has a lower sensitivity than other methods
- should be confirmed by a blocking test or another method
- is not suitable for Test of Cure (TOC)
Other Methods
- Ligase chain reaction (LCR) or polymerase chain reaction (PCR)
- These methods are used to detect nucleic acid (DNA) by amplification techniques and are used for testing urethral, cervical or urine samples but are not often used for Lymphogranuloma inguinale.
Note Screening for other possible causes of genital ulcerative disease should be carried out, such as for:
- HIV
- Herpes simplex
- Haemophilus ducreyi
- Klebsiella/Calymmatobacterium granulomatis
- Serological syphilis
- Treponema pallidum
Lymph node biopsy may be used to make differential diagnoses with atypical infections and neoplasia.
Lymphogranuloma Treatment
Lymphogranuloma inguinale is a very persistent bacterium, and penicillins are ineffective in treatment because they can suppress the bacteria without killing them. Early treatment is essential to reduce the severity of the chronic phase. A 3 week program of antibiotics is recommended to kill the infection.
Antibiotics used:
- Azithromycin
- Chloramphenicol (effective against Chlamydia trachomatis)
- Doxycycline
- Erythromycin
- Isulfamethoxazole
- Minocycline
- Rifampicin
- Sulfadiazine
- Tetracycline
Patients allergic to Cyclines should be treated with Erythromycin.
Follow-Up
- patients should be followed clinically until signs and symptoms have resolved.
- pregnant and lactating women should be treated with Erythromycin.
Note In HIV patients:
- delay in healing may occur
- development of multiple abscesses can occur
- latent Lymphogranuloma inguinale may be reactivated
- prolonged therapy may be required
Lymphogranuloma Prognosis
Complications
- A burst bubo can take months to heal completely and often leaves a deep scar or a hard mass of scar tissue
- Buboes may ulcerate and discharge pus from multiple points creating chronic fistulas
- Inflamed, swollen lymph glands may drain and bleed
- Spontaneous remissions and exacerbations can occur usually within 8 weeks after treatment
- Surgery may be needed to repair the internal and external scars and erosions caused by advanced infection
The systemic spread of Chlamydia trachomatis may be associated with:
- arthritis
- fever
- peri-hepatitis
- Pneumonitis
Stage 3 Most people recover after the secondary stage without any complication. In a few cases, however, mostly among women, the persistence and progressive spread of Chlamydia trachomatis in anal-genital tissues will cause chronic inflammation and destruction of tissues, which can lead to:
- acute Proctocolitis (symptoms similar to Crohn’s disease)
- chronic granuloma, a disfiguring condition of the vulva
- fibrotic lesions (fibrous tissue that develops in response to the irritation)
- fistulae (abnormal connections between an organ or vessel and another structure)
- proctitis (inflammation of the anus or rectum)
- strictures (narrowing of tubes such as the urethra)
- surgical repair, including reconstructive genital surgery may be necessary
If left untreated the following problems can occur:
- an association with rectal cancer
- destruction of lymph nodes
- elephantiasis (extreme swelling) of the genitals
- persistent suppuration (formation and discharge of pus)
- pyoderma (purulent skin disease)
- rectal or intestinal blockages
- scarring
- serious tissue damage
- the central nervous system can be attacked
Lymphogranuloma Prevention
- avoid unprotected sex until treatment and follow-up have been completed
- carefully wash genitals after sex
- if infected abstain from sex until the infection is cured
- if you think you have come in contact with Lymphogranuloma inguinale contact your local STD clinic, health professional or urologist immediately
- use latex condoms put on before sex and worn until the penis is withdrawn
- limit sexual relationships to a single, uninfected partner
- notify all sexual contacts immediately so they can obtain examination and treatment
Note Before having sex it is advisable to check for anything unusual in your partner, such as:
- discharge
- rashes
- sores
- swelling
Douching or urinating after sex does not prevent STDs. If you have had sexual contact with a person infected with Lymphogranuloma inguinale within 30 days before onset of the person’s symptoms you should be:
- examined
- tested for urethral or cervical chlamydial infection
- treated if the infection shows up in tests
- receive presumptive treatment